Chronic peripheral arterial disease of the lower extremities, is defined the disturbance of the blood supply as a result of damage (stenosis-blockages) in the arteries of the legs. The progressive and worsening blood flow disorder over time usually manifests as pain during walking (intermittent claudication), while in advanced stages it can be expressed by constant pain in the lower extremities (pain at rest) or gangrene. In the majority of patients, the cause of peripheral vasculopathy is atheromatosis (arteriosclerosis), i.e. the set of changes in the walls of the arteries, as a result of chronic tobacco use, diabetes mellitus, increased cholesterol and arterial hypertension.
Recently, in a clinic in our city, we encountered a special case of peripheral arterial disease of the lower extremities, in a young patient with a history of chronic tobacco use. The patient presented with severe leg pain during walking, which forced her to stop after a distance of 20 meters. Both the investigation and the therapeutic approach to the incident were carried out at the clinic by specialized personnel.
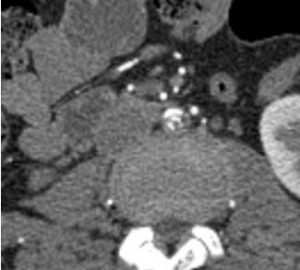
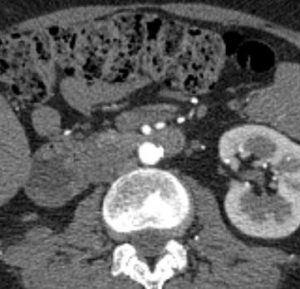
The patient underwent CT angiography, which diagnosed localized, high-grade atherosclerotic abdominal aortic stenosis (80%) more central to the aortic bifurcation (img. 1,2). Due to the rare localization of the lesion, the young age of the patient and the history of previous abdominal surgery, the minimally invasive endovascular technique was decided as a method of treatment. It was also deemed necessary to inform the nephrology department and the artificial kidney unit of the clinic, for their possible intervention, in case of kidney dysfunction, due to the intraoperative administration of contrast (the patient has only one functioning kidney).
The endovascular intervention was performed by inserting guide wires through the femoral arteries (right and left). Under continuous fluoroscopy (C-ARM), two stents (STENS) were advanced into the aortic lumen to penetrate the lesion area. The stents were precisely fixed and deployed, centrally at the level of the suprastenosis and distally to the common iliac arteries (Crossing Balloon Technique). The final expansion (balloon expansion) of the innards resulted in the destruction of the atheroma and the complete restoration of the blood supply to the lower limbs. The patient remained in the clinic for follow-up and was discharged ambulatory and in excellent condition on the first postoperative day.
The success of vascular interventions (surgical-endovascular) depends on the experience of the vascular surgeon, who, with the support of the appropriately equipped center, provides the safest and best possible treatment to each patient. Following the developments in the field of vascular surgery and having ensured the above conditions, we are now able to manage, in treatment centers in our region, cases of high demands, which could not previously be treated at a local level.
Ioannis L. Mazarakis
Military Physician-Vascular Surgeon Master of Science in Endovascular Techniques Postgraduate Trained in Vascular Ultrasound
Professor candidate of the University of Athens, Scientific Associate of Anassa General Clinic